MHAOK is honored to have Dr. Xavier Amador as our first keynote speaker of the 2023 Zarrow Mental Health Symposium: New Horizons in Brain Science. His presentation aptly shares a name with his best-selling book, “I AM NOT SICK! I don’t need help!” It was compelling, educative and filled with ‘aha moments.’
Like most good speakers, Dr. Amador began on a personal note. He shared his experience of losing his biological father in the Cuban Revolution and the subsequent escape he, his three siblings and widowed mother on the heels of that tragedy.
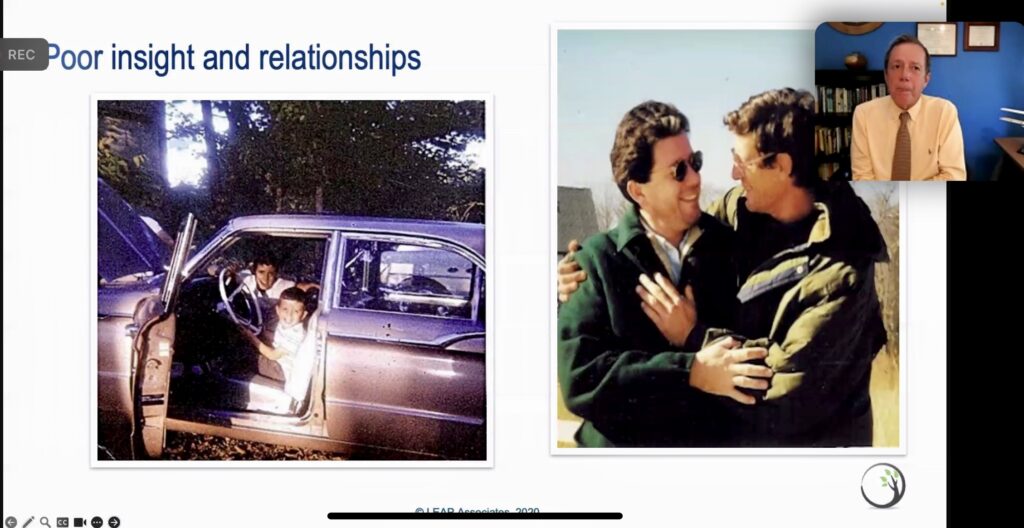
It was precarious for them, Dr. Amador said, but they were able to cultivate very rich and full lives that included welcoming a loving stepfather into the family. He told us of his brother, Henry, who, in his twenties, began exhibiting signs of schizophrenia.
It was 1981 when Dr. Amador, a senior in college, received a frantic call from Henry insisting that he killed his stepfather and Dr. Amador needed to come home to Tucson. Henry had been playing the guitar and believed that the music had been transmitted into his stepfather’s head, causing him to trip, fall and die of a head injury.
Their stepfather died of a heart attack while on a jog.
This began a seven year cat-and-mouse relationship – Henry, the mouse, and family, friends, doctors, all the cats. Henry experienced a stint of homelessness, remained unemployed and was hospitalized an average of four times per year, often involuntarily. Eventually, Henry figured out that he could voluntarily admit himself and be discharged more quickly by “agreeing” that he had an illness.
That changed, one day, when Dr. Amador was in training to become a clinical psychologist. He was working with a female patient on an in-patient ward who behaved so similarly to his brother. Convinced there was nothing he could do, he went to his supervisor to lobby for her transport to the state hospital.
His supervisor pressed pause, directing him to ask his patient what she wants, to ask her what her goals are. “Stop telling her she has a mental illness,” his supervisor said. “Stop telling her she needs to take medicine.”
And so he did.
When his patient expressed that she wanted out of the hospital and for her mom to stop calling the police, he committed to working with her on those goals. Within a few weeks, she accepted medication and moved from hospital submission to clinical care. Perhaps this was the better approach for his brother?
Dr. Amador went to his phone.
He apologized to Henry for insisting he was mentally ill, for insisting he take medication. He promised not to repeat those mistakes and instead, he pivoted to a collaborative approach – one rooted in compassion, in empathy.
That shift from educating his brother to listening and working with his brother – a shift that did not include his brother understanding he had a mental illness, by the way – was the difference maker. Within six months, Henry was on a long-term injectable and on his way to a fulfilling life, rich with community. His relationships served as an impetus to remain on medication, and he thrived in both for the next eighteen years until a car wreck took his life.
This story of humanity, of tragedy, of resilience and of compassionate perspective is the foundation for the LEAP method and its profoundly effective approach to assisting those living with anosogosia.
Anosognosia is a symptom of severe mental illnesses (SMI) such as schizophrenia, bipolar disorder and borderline personality disorder that renders someone unaware of his or her illness. It predisposes the individual to noncompliance with treatment, leading to higher relapse rates, increased number of involuntary hospital admissions, poorer psychosocial functioning and a poorer course of illness. This neurocognitive symptom can be confusing and frustrating for loved ones or caregivers, but it is not an impossibility. It is not hopeless.
The LEAP method is an evidence-based practice designed to create alliances and engagement with individuals who live with SMI. It consists of seven communication tools used in the context of an overall engagement strategy, and these tools are derived in part from Client Centered Therapy (CTT), Cognitive Behavioral Therapy (CBT) and Motivational Interviewing/Enhancement Therapy (MIT/MET). The seven tools are:
L (listen): Hear all of what the individual has to say and reflect back without judgment, reactions or contradictions
E (empathy): Express empathy for feelings coming from delusions, anosognosia and desires
A (agree): Find areas you can agree on and abandon your goals of getting the person to agree to a mental illness
P (partner): Move forward together to achieve common goals
D (delay): Pause on giving hurtful and contrary opinions, rather redirect and ask permission
O (opinion): Then give your opinion with humility and respect
A (apologize): Show remorse for acts and interactions that may have felt disrespectful, frustrating or disappointing
No amount of education, no amount of experience changes the fundamental truth that a person with anosognosia holds. The individual often feels betrayed, depressed, suspicious and lonely when others try with insistence to educate an individual on his or her mental illness. Collaboration is the goal.
Dr. Amador’s presentation was insightful from his first word to his last, and his message could be summarized for lay people and clinicians alike: We don’t win by the strength of our argument, but by the strength of our relationship.